Who Me?
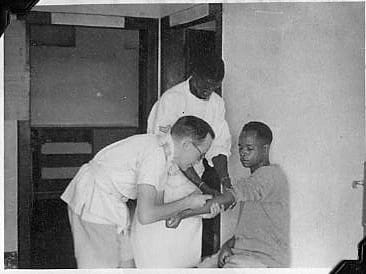
Dad had a lot of experience treating Africans from South Africa all the way north to Abyssinia before he settled in Que Que
Who Me?
As I mentioned in my last blog Mrs. Tyzack handled the WWII ex-ambulance with great aplomb on the weekends. During the week she was my dad’s indispensable nurse at his surgery, Stanley House, coping with all of his foibles.
Who Me?
She was wiry, spare in every way, except for a square smile that revealed widely spaced teeth. Dad coaxed her into running BUN’s and sugars (blood urea nitrogen and blood sugars) and even hemoglobin’s amongst other things in a small laboratory my fiancé and I set up there after I joined Harare Hospital in Salisbury. Despite her protests “I am a nurse not a medical technologist”, she was good. In the afternoons she would occasionally stand-in for Cookie in interpreting at the native clinic in the back of the surgery. She could speak Fanagolo, a pidgin language of Zulu, English and Afrikaans.
Dr. Gelfand had been instrumental in encouraging Dad to come to Rhodesia. They had become close friends. He stayed in his house during the week for the first six months of his Parliamentary term before he bought a house in Salisbury. But he did not share Gelfand’s fascination and empathy for the cultural differences between Europeans and Africans in response to disease. He was imbued with the effectiveness of Western medicine, especially with the advances following WWII.
Africans attribute illness to supernatural causes, believing the cure is also supernatural. The African feared that by consulting a white doctor he further provoked the spirits of his ancestors. The lack of patient confidence, Gelfand explains in his tome The Sick African ‘is practically impossible to overcome’ and ‘lack of cooperation with the white doctor one of the great difficulties of Native practice.’ Dad was enthusiastic about his ability to diagnose disease and dispense Western medicine. He did not address the African cultural deficiency.
Mrs. Tyzack could curb Dad’s impatience with African traditional lengthy greetings and primitive evasiveness when there were forty or fifty patients to be seen in an afternoon. The conversation would begin something like this:
“Kunjani?” (How are you?) What’s the trouble here?”
“I am well. How are you.”
“Do you have a pain?”
“Who Me?”
“Yes, you! Who do you think I am talking to?”
“Yes Nkos.”
“When you get the pain, where is the pain?”
“I am well.”
“What’s the trouble?”
“I need a certificate.”
“I can’t give you a certificate if you are not sick. What is the trouble?” he would say testily. Mrs Tyzack would be checking the vital signs: pumping up the blood pressure cuff, checking the pulse rate as the second hand on her man’s wrist watch ticked on.
“Say ah”, he’d say, as he thrust a tongue depressor down the throat, before the patient could ask ‘Who me?’
The conversation would be interrupted as he listened to the heart, the chest front and back.
He palpated the abdomen, and the lymph nodes under the chin and neck.
While she interpreted and soothed both parties, he’d be noting the whites of the patient’s eyes. Was he jaundiced? He’d flash his penlight to examine pupil response and ocular motion.
He’d pull down the eyelids, was he anemic? A quick look with the auroscope at the ears. Quick taps to record reflexes.
“Does it hurt here or there?” he would ask as he palpated the abdomen.
“Yes, Nkos,” again answering a factual question with African politeness.
“Ask him, Mrs Tyzack”.
He would pull up the stethoscope and slap the diaphragm on the abdomen and listen carefully for bowel sounds.
He’d move on to the extremities, looking for clubbing, cyanosis and edema.
He’d remind himself that not only did tropical diseases plague them, but a host of others could present in combination: pneumonia, TB, syphilis, gonorrhea, heart disease to name a few. Generally, they were so much sicker than the Europeans on whom he lavished fifteen to thirty minute appointments in the mornings, although often the problem could be attributed to overindulgence of one sort or another. But the people in his mornings shared the same culture, understood the same facts and had confidence in them, with the same expectations. It was tragic the African didn’t have the where-with-all to reject his own culture, and when they did they were conflicted. The press of numbers in the face of such sickness made him testy. If he did not keep his impatience in check, Mrs. Tyzack would reassure the patient and pull him up short.
It was all over in a matter of minutes. “Sit up,” he would say. He’d leave Mrs. Tyzack to give instructions. They maintained a free lab and pharmacy service on the premises. Finally she’d stress the importance of coming back.
“Who me?”
